The Pervasive Addiction




Alcohol ruined me financially and morally, broke my heart and the hearts of too many others. Even though it almost killed me, sometimes I wonder if I could get away with drinking some now. Alcoholism is a mental illness because thinking like that is clearly insane.
— Craig Ferguson, Comedian
Alcohol Use Disorder or AUD is indiscriminate in its demographic reach, affecting people of all races, age, social and economic class, education, and gender, due to the singular reason that it, unlike other drugs, is legal. Its legal status accords tolerance to drinking and normalizes and erases the stigma of overconsumption. It is viewed as a glue for social bonding and fellowship, and as a ritual to mark celebrations including healthy, wholesome activities such as sports. Drinking is so ingrained and socially acceptable in our culture, that those who abstain from alcohol are the ones considered different and unconventional.
As alcohol manufacturers and purveyors actively market their products to persuade and convert non-drinkers to use alcohol, the number of Americans afflicted with AUD has risen. Alcoholism ranks behind nicotine as America’s leading addiction. Those most susceptible to the lures of alcohol are youth between the ages of 14 to 24.
AUD is a persistent, progressive disorder marked by an overpowering compulsion to use alcohol, an inability to control the amount consumed, and the necessity to drink to feel emotionally stable and positive. Afflicted individuals feel powerless to cease drinking despite its negative effect on their health, relationships, work, and school. Mild, moderate, or severe AUD is diagnosed when a person meets any 2 of 11 DSM-5 criteria over a 12 month period.
The general acceptance of drinking makes alcohol a highly profitable commodity for manufacturers and purveyors. In 2019, domestic alcoholic beverage sales reached $253 billion. The industry spends over $3 billion each year marketing liquor to Americans, half that amount on advertising. The rest is spent promoting the benefits of alcohol at music festivals, sports events, spring break, movie theaters, billboards, and social media. The goal of alcohol marketing is to protect market share from competitors, persuade people to switch brands, introduce new products, and most importantly, to attract new users—mostly young people.
The industry spends a further $42 million annually lobbying state legislatures and donating to members of Congress. More than 300 professional lobbyists for the industry work in Washington DC. The result is the complicity of politicians, who otherwise oppose illicit drugs, pontificate about opioid addiction, and rave about punishing drug traffickers with the death penalty.
Alcohol advertising to youth is strategically designed to persuade and groom young people to drink. The Center on Alcohol Marketing and Youth at John Hopkins Bloomberg School of Public Health found a pattern of alcohol advertising in magazines that had disproportionately youthful readers. Routinely, the ads glamorized drinking. The ads linked drinking to fun and good times, showed drinking near activities requiring concentration and coordination such as water sports, highlighted high alcohol content in products, equated drinking with popularity, and presented sexualized messages. Alcohol advertising in social media is also pervasive and designed to engage young people to interact with the messages through views, clicks, shares, and comments.
The numbers point to an urgent public health epidemic looming over the horizon. More than 18 million American adults suffer from AUD—75% men and 25% women. AUD is the leading cause of preventable death among adults, killing 75,000 men and 25,000 women each year.
Alcohol’s impact on kids is even more serious. More than 131,000 kids age 12-17 were arrested for liquor law violations in a year. More than 400,000 kids suffer from Alcohol Use Disorders—300,000 girls; 100,000 boys. Each year, nearly 5000 youth under 21 die in alcohol related deaths in car crashes, homicides, or suicides. For kids, drinking is a precursor to other problems including other drugs, risky activity, sexual activity, mental and emotional disorders, and future alcoholism.
Binge drinking refers to excessive drinking in a short period—5+ drinks for men and 4+ drinks for women. The group most likely to indulge in binge drinking are American youth, mostly college students. Additionally, more than a third of college students nationwide engage in extreme drinking—10+ drinks for men and 8+ drinks for women.
The dangers of binge and extreme drinking go beyond progressive harm to physical health. According to a recent survey by the National Institute on Alcohol Abuse and Alcoholism, in addition to fatal outcomes, nearly 700,000 students age 18-24 had been assaulted by drunk students, 97,000 had been victims of alcohol-related sexual assault or date rape, and a quarter of AUD students reported a slew of problems including academic failure and absence.
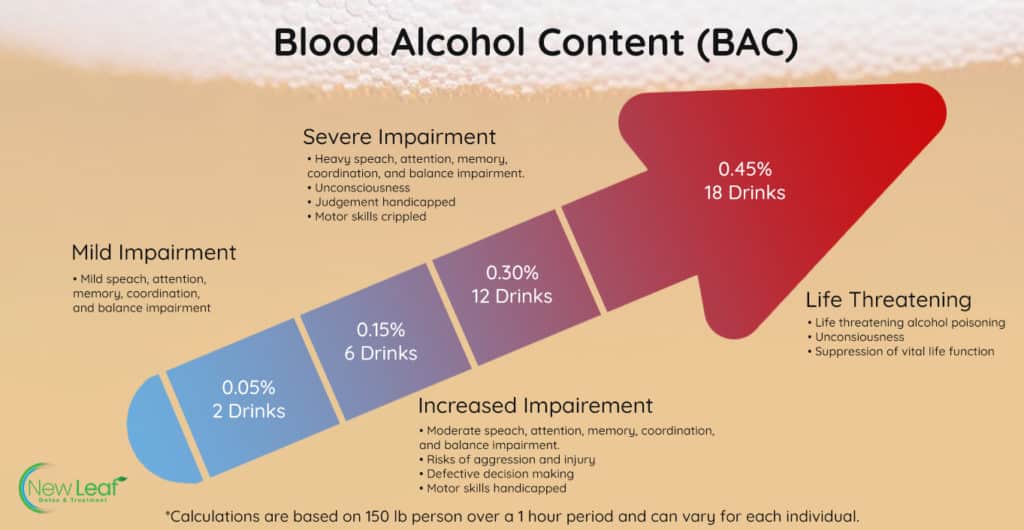
Binge and extreme drinking cause dangerous amounts of alcohol to surge through the bloodstream, forcing the shutdown of vital organs and functions. Alcohol poisoning and overdose can result in choking and vomiting, hypothermia, respiratory and heart failure, seizures, loss of consciousness, and death.
Knowing the alcohol content of drinks can help us avoid binge and extreme drinking. The highest alcohol content is found in undiluted distilled spirits such as gin, vodka, whiskey & tequila, while wine has less, and beer has the least.
Each of the following equals one “drink.”
If you suspect that you or someone you love is grappling with drinking, please take this audit to confirm symptoms and consult your primary care physician.
Most of us are aware that alcohol abuse can result in liver damage, and that excessive drinking can cause injuries, accidents, and fatal car crashes.
The most vivid examples of alcohol’s danger to the body, however, are the litany of alcohol-related deaths of college students in fraternity hazing rites. The 2017 death of Penn State U. sophomore, Tim Piazza, is a shocking, cautionary tale about alcoholic poisoning. During hazing, the 19-year-old was forced to drink 18 alcoholic drinks in 82 minutes. On an empty stomach and anti-depressants,
Tim was quickly intoxicated, fell down a staircase, and was rendered unconscious. He regained consciousness several times throughout the night, staggered to walk, crashed into an iron railing, and fell on a stone floor.
Hours later, Tim was taken to hospital with a lacerated spleen, an abdomen full of blood, hemorrhagic shock, and multiple traumatic brain injuries. Almost half his skull had to be removed to relieve the pressure on his swollen brain. His blood alcohol content was 0.40, a level that guaranteed death.
The effects of alcohol on the body accrue and contribute to a range of threats to physical health. They are a contributor to serious harms including fetal alcohol disorders, cardiovascular diseases, liver cirrhosis, cancers, hypertension, stroke, type 2 diabetes, mental health disorders, and accidental injuries.
Spikes blood pressure, increases risk of stroke & congestive heart failure, changes heart beat.
Inflames stomach lining & causes pain.
Represses bone marrow, lowers white and red cell & platelet counts.
Lowers immunity to a host of diseases.
Affects cognition and muscle coordination. Slurs speech, blurs vision, decreases reflex & reaction. Causes memory loss, increases risk of dementia, and fuels anxiety and depression.
Increases risk of mouth, throat, esophageal, breast, liver, and colorectal cancer.
Depletes ability of the liver to rid itself of fat as it diverts attention to rid body of alcohol.
Lowers hormones that enable circulation of water to the body.
Wreaks havoc throughout the network including slowing and stopping breathing. Memory making portion of the brain that creates blackouts.
Disclaimer: Only for fair use for educational purposes and illustration. We do not own the copyright to this video.
While the responsibility of committing to recover from alcohol addiction falls solely on those afflicted by the disorder, it is important to consider AUD in the context of contributing factors.
Your genetics, heredity, family, culture, and friends do affect your vulnerability to AUD. Parental neglect, poverty, adverse childhood experiences such as abuse or trauma, family members who drink, access to alcohol, and peer pressure all heighten the risk of AUD. Conversely, good parenting, stable family, and nurturing caregivers, relatives, teachers, and mentors can protect a person predisposed to AUD from affliction. Research has found that genes are at least half the reason why a person is susceptible to the disorder. Undiagnosed disorders such as depression, bipolar, ADHD, and anxiety may also compel people to self-medicate with alcohol.
But, AUD does not need to be a person’s inevitable fate. Despite genes and environment, or nature and nurture, learning behaviors to manage the risk can prevent a person from falling victim to this voracious addiction.
While the desire and commitment to stop or limit drinking rests entirely with AUD sufferers, recovery from AUD requires the treatment, support, and care of others. Rare is the AUD sufferer who can recover alone.
The type of treatment depends on the severity of the disorder and the circumstances of the afflicted person. A single mother of young children with moderate AUD may need an outpatient treatment plan, while a college student crippled by severe AUD who has good health insurance coverage would benefit from a residential program. Regardless of individual circumstances, the first conversation should always be with your primary care physician.
After evaluation with AUD, the most severe cases may require a program that begins with Detox under the care of clinicians. Withdrawal from alcohol is a painful process with symptoms including nausea, vomiting, headaches, tremors, confusion, anxiety, hallucinations, delusions, heart palpitations, and seizures.
The fear of withdrawal can keep many people chained to their addiction. Detox with Medication Assisted Treatment (MAT) under clinical supervision can alleviate or lessen withdrawal symptoms.
Recovering from AUD requires an array of learned skills and managed behaviors. Few people can navigate recovery without the help of behavioral health professionals.
Trained professionals can help patients identify situations, people, and behaviors that trigger drinking, and help them reframe and manage the triggers. They can fortify those in recovery with support, motivation, goal setting, and techniques to relieve stress, develop resilience, and help them envision and forge a new alcohol-free identity.
AUD sufferers will find group counseling and peer support such as Alcoholics Anonymous essential to their education and healing, and critical to their goal of thriving and flourishing without alcohol. The afflicted person and his immediate family who have been affected by the patient’s AUD may need joint counseling, such as marital and family counseling.
Families may also wish to join peer support groups such as Al Anon to help them care for themselves and support their loved one.
New Leaf Detox & Treatment meets the needs of AUD patients with the most advanced best practices in addiction treatment and evidence-based standards of care, while mindful of each client’s individual needs.
After extensive patient-provider engagement, careful screening, and medical and psychological evaluation, the clinicians create a treatment plan specifically designed for the patient. With severe AUD, the patient may require Detox accompanied by Medical Assisted Treatment (MAT). By utilizing a controlled taper of MAT—of either Lorazepam (brand name Ativan), Phenobarbital, or Librium—the patient can gradually become used to living without alcohol.
These medications help diminish cravings, manage anxiety, reduce high-risk behaviors associated with substance abuse, and create stability for patients to prevent relapse. The patient is closely monitored by a doctor or clinician throughout MAT treatment.
After Detox, the patient begins cognitive-behavioral treatment plans tailored for the patient. They include individual counseling, group counseling, anxiety focused therapy groups, and process groups and activities. The primary clinician and individual therapist and group counselor work in concert to treat the patient by resolving the underlying issues that led to addiction.
This is followed by a variety of custom treatments that fortify the patient, clinical assessments throughout the process, and a considered discharge plan. Peer support, onsite medical assistance, family involvement, and post-treatment follow up support are part of New Leaf’s standard of care.
For more information about New Leaf Detox & Treatment, please contact us at 1-866-932-0905 or email us at info@nldetox.com.