Opioids: The Deadliest Addiction
Treatable With Early Intervention
2020 saw the highest number of opioid-related drug overdose deaths since the first wave of opioid-induced deaths on the West Coast in the early 1990s. According to CDC’s provisional data reporting, more than 87,000 Americans died in the year ending September 2020.
The leading cause of drug overdose deaths were opioids such as fentanyl and its variants, followed by toxic cocktails of heroin and cocaine spiked with fentanyl and fentanyl analogs, methamphetamine, cocaine, and other psychostimulants, and prescription drugs.
Opioids, both semi-synthetic pharmacological formulas prescribed by physicians, and extremely potent illicit manufactured fentanyl are highly addictive. But opioid addiction need not be a death sentence. Early intervention and customized, individualized treatment plans designed for those suffering from opioid use disorders are the key to safe detox, overcoming addiction, and avoiding relapse.
Physicians and their medical and clinical specialists in addiction medicine and treatment are able to design drug rehab plans as unique as each individual and the specific opioid they are addicted to. Individualized plans can include Medication-Assisted Treatment (MAT) during detox, and after detox for maintenance, together with individual and group therapy, and social support groups.
Due to the diversity and varying sensitivity of patients’ biology, mental and physical states, tolerance, and effects of the type of opioids used and the medications prescribed to address the addiction, caregiving teams and medical case managers constantly examine, monitor, evaluate and discuss the patient’s progress. MAT protocols and dosages are refined, adjusted, increased, decreased, or changed as needed.
Effects of Opioids
Opioids are mind-altering, psychoactive chemicals that activate and trigger neurotransmitters in the brain responsible for positive feelings and pleasure. Opioids cause a surge of endorphins that subdue or extinguish pain, and create feelings of pleasure and euphoria. In the central nervous system, they attach to opioid receptors in the brain that control pain and emotions, and mimic the way naturally occurring pain relieving chemicals in the body soothe or alleviate pain. In the peripheral nervous system, they attach to opioid receptors in the cranial nerves, and the spinal and peripheral nerves roots and branches. They also attach to the neuromuscular junction, the synapse connecting nerve to muscle that activates motion and physical action.
Opioids relieve pain, relax the body, and make users feel happy and euphoric. The flip side of opioid use is a litany of negative side effects from minor to deadly. They can make people drowsy, dizzy, confused, and nauseous. The relaxant effect also slows respiratory function, and may cause vomiting, unconsciousness, coma, and death.
Origin of Opioids
The most natural form of opioids are extracted from plant resins such as opium poppy. In this form, they are called opiates and mostly used for medicinal and pharmacological purposes. Semi-synthetic opioids are pharmacological lab formulations that combine opiates and lab chemical compounds with similar structures as opiates. These formulations are for medicinal use that are prescribed by physicians to patients. Synthetic or manufactured opioids are illicitly manufactured street drugs made entirely from lab chemicals. They are extremely potent and sold in pure form, or frequently used to bulk up heroin, cocaine, and other street drugs in toxic cocktails.
Opiates
This class of opioids are naturally occurring base chemical compounds containing nitrogen—alkaloids withdrawn from the resin of the opium poppy. In this pure state, the harvested opium, morphine, codeine, and thebaine are called opiates. In their pure form, they are reserved for medical, pharmacological, and pharmaceutical use.
Semi-synthetic Opioids
In the lab, opiates are combined with chemicals to formulate semi-synthetic opioids—prescription medications such as hydromorphone, hydrocodone, and oxycodone, and codeine. Heroin is also a semi-synthetic opioid formulated with morphine and lab chemicals.
Synthetic/Manufactured Opioids
Fully synthetic or manufactured opioids are free of any naturally occurring opiates. These lab-originating opioids are extremely potent. They include fentanyl, fentanyl analogs such as carfentanil, pethidine, levorphanol, methadone, tramadol, and dextropropoxyphene.
Risk of Addiction to Opioids
Prescription opioids are dispensed for moderate to severe pain. Because opioids attach to receptors in the pleasure and reward centers of the brain, people who take opioids even for a short duration can quickly develop a craving for more to repeat the experience of pleasure and painlessness. Those who need the drug for these reasons are willing to gamble their lives to attain the positive feelings of opioids, while hoping they can avoid the worst negative and even deadly side effects. But opioids are so powerful that anyone taking them, in any of the three variations, is vulnerable to developing an addiction.
Developing Tolerance to Opioids
Due to the opioid crisis, physicians are more careful about prescription opioids such as oxycodone, hydrocodone, and fentanyl. The surge of endorphins activated naturally in the body are compromised and slowed down with repeated opioid use. Individuals who are tempted to recreate the initial feelings of euphoria they experienced during the first days of opioid use, will increase the dosage of opioids as they develop a tolerance for the substance.
The duration of prescribed opioid use influences future dependence and addiction. Using prescribed opioids for even a few days is a factor in dependence and addiction. Research shows that five days of use can increase the risk of dependence by one year. Opioids are so highly addictive that most users develop tolerance and keep increasing their intake in order to sustain base levels of feeling good. Chasing the first high after increased opioid use over a period of time will require larger and larger quantities that could lead to the most serious side effects including coma and death.
Opioids are potent to begin with. When taken in forms other than the one prescribed, for example, turning a pill into a powder to inject or snort, the opioid becomes lethal. Both the potency of opioids and extended release make them dangerous and deadly because of intense rapid delivery to the body.
Turning to Street Opioids
In the face of the opioid epidemic that has caused the deaths of half a million Americans since the 1990s, doctors have become more aware of the addictive nature of opioids. Ethical doctors now limit opioid prescriptions to less than a week and are reluctant to renew prescriptions. Cut off from prescription opioids, patients who develop a dependence to the prescribed substance inevitably turn to the street to secure a supply of their drug of choice or drugs that emulate the effects of the opioid prescribed by their doctor. On the street and online on the dark web, drug dealers offer an array of opioids and opioid cocktails. The list of illegally manufactured/synthetic street opioids available across the US is long.
Street opioids are cheap to manufacture, cheap to acquire, and uncontrolled in their formulations, frequently contaminated, or cut with dangerous chemicals that increase the already high potency of opioids. Street opioids and cocktails of opioids are the leading cause of drug overdose deaths followed by prescription opioids in combination with other drugs.
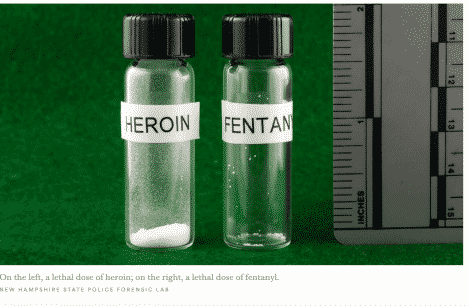
According to a frontline report from New Leaf Detox & Treatment in San Juan Capistrano, CA, street opioids are dangerous to humans because of their potency. “Before fentanyl, from the 1960s to 1990s, street drugs were sold and ingested in grams. It was common for people to use 1-3 grams of heroin a day without overdosing or dying. Now opioids like fentanyl and carfentanil, due to their extreme potency, are sold and used in micrograms. One microgram is one-millionth of a gram. People are dying using 2 to 5 micrograms of fentanyl that cost $5. Fentanyl is 50 to 100 times more potent than morphine, and Carfentanil, an elephant tranquilizer that is 10,000 times more potent than morphine, can be purchased on the street for less than $10.”
Lethal Doses of Heroin and Fentanyl
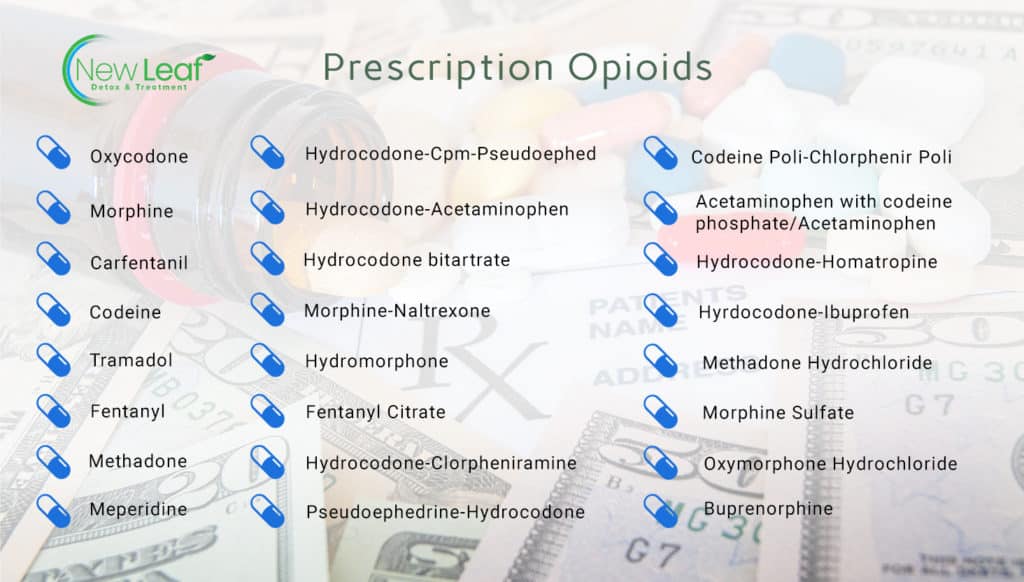
List of Prescription Opioids
Synthetic Street Opioids
Though there are some synthetic prescription opioids, illegal synthetic opioids are manufactured in China, Mexico, and elsewhere and imported to the US or sold on the dark web. Most are fentanyl and fentanyl analogs sold alone, or used to cut and bulk up heroin, or combined in cocktails. They are sold either in powder or crystal form or as replicas of prescription opioids in pill form. People either sniff the powder from blotters, or use them in eye drops or nasal sprays, or in capsules. Many Americans die each year from deadly cocktails of heroin, cocaine, methamphetamine, and MMDA, spiked with cheap fentanyl by drug dealers to bulk up the mixture.


Opioid Overdose
It is often difficult to specify which drug is responsible for an overdose because drug suppliers add cheap fentanyl to drugs to produce more intense highs and for profit by bulking up expensive heroin and cocaine with fentanyl.
During an overdose, the brain and body are flooded with very potent opioids that give the user an explosive high. The user’s breathing slows down, heart rate decreases, and alertness fades. The brain is deprived of oxygen during this dangerous period of decreased breathing and heart rate. The user will quickly go into cardiac arrest, brain damage, coma, and death due to respiratory malfunction.
Life Saving Overdose Reversal Medication
But opioid drug overdoses, if caught in time, can be prevented with drug overdose reversal medication. Naloxone (traded as Narcan or Evzio) is an antagonist that binds to opioid receptors and blocks or reverses the effects of other opioids. When given in time, it can quickly restore and normalize breathing and heart rate. FDA approved Naloxone is available in three formulas. The first is an injectable that requires training and assembly. It is intimidating for non-medical professionals with no experience, or who feel nervous giving injections.
The less intimidating iteration is Evzio, an auto-injection that is already filled with Naloxone. When activated, the device provides audio instructions to those offering aid on how to deliver the medication, similar to auto-defibrillators. The injection is administered to the outer thigh area. The most user-friendly Naloxone for those with no medical training, who are nervous about injections, is the Narcan nasal spray that is sprayed into one nostril while the opioid user is lying on his/her back.
Withdrawal from Opioids
The side effects of stopping opioid use, suddenly on your own without professional medical assistance can be intense, severe, and painful. Withdrawal symptoms include muscle and bone pain, flu symptoms, fever, diarrhea, vomiting, fatigue, insomnia, anxiety, cold flashes, shivers, uncontrollable limb movements, cravings, and migraine. Under professional medical supervision, detox can be a safe, slow-tapering process that gradually decreases opioid dependence, most often with detox medications.
Medication Assisted Treatment for Opioids
The gold standard of care in treating opioid addiction is evidence-based Medication-Assisted Treatment (MAT), a disease management model that strives first for patient stability through medication assistance, then as a launchpad for recovery, and finally as an integral tool in a comprehensive treatment plan unique to each individual. During the transitional period from opioid dependence to opioid abstinence, MAT allows the patient to detox from opioids in a safe way under medical supervision without drastic outcomes but in a slow taper. MAT detox regulates brain chemistry and biological functions, relieves the symptoms of withdrawal from opioids, diminishes cravings, and improves a person’s ability to function normally.
Custom-designed MAT plans at a licensed and accredited drug detox and drug rehab—such as those offered at New Leaf Detox & Treatment in San Juan Capistrano—that include medication for detox and maintenance, psycho-social support, and behavioral health modules enable those who suffer from Opioid Use Disorders (OUD) to stay engaged in programs for the long term, significantly lowers a return to opioid use, increases immunity against relapse and overdose, and substantially increases the odds of sustained recovery.
When added to the arsenal of conventional treatment and wraparound support services, MAT is an exemplar in care for opioid use disorders. It has the capacity to address the chronic disease according to each patient’s needs. Several studies show that MAT reduces the likelihood of relapse and overdose fatality significantly.
FDA-Approved MAT
The three FDA-approved MAT drugs for heroin and opioid dependency are Buprenorphine, Methadone, and Naltrexone.
Buprenorphine
Buprenorphine is a partial opioid agonist, that at low to moderate rates mimics similar but low grade effects of opioids such as euphoria or respiratory depression. It also blocks the effects of other substances. Since it is a long acting agent, it allows patients to have intervals in regimen. It diminishes withdrawal symptoms and cravings, and lowers the risk of misuse and danger of overdose. It is prescribed as a tablet, cheek patch, or six-month implant under the skin. It is prescribed in the doctor’s office after screening and evaluation.
Methadone
Methadone is a synthetic full opioid agonist that activates the same receptors in the brain that other opioids such as heroin and morphine do, but at a slower pace. It does not produce euphoria, but does reduce opioid craving and withdrawal and blocks the effects of opioids. It is a long lasting agent, taken once a day, and is available as liquid, powder, and tablets. Methadone is only dispensed in specialized treatment programs and clinics.
Naltrexone
Naltrexone is an opioid antagonist that prevents the effects of heroin, opioids, and alcohol on the brain by blocking opioid receptors. It is non-addictive, does not mimic the effects of other opioids, and prevents full relapse or overdose by other drugs because of its antagonist properties. The earlier pill form has been replaced by an extended-release monthly injectable, Vivitrol, which has proven effective in MAT. While Naltrexone is not as effective for heroin and opioid treatment alone, in combination with buprenorphine it is an effective treatment. Its use for successful treatment is supported by multiple scientific studies.
MAT when coupled with counseling is the most effective current treatment available for opioid addiction disorders.
Opioid Addiction Treatment at New Leaf Detox & Treatment
New Leaf Detox and Treatment offers client-focused customized detox and treatment plans customized for patients and as individual as each client. Using the latest advances in addiction medicine and science, New Leaf offers levels of care that address the complexity of opioid use disorders from dual diagnosis to trauma-informed care.
Our Medication-Assisted Treatment practitioners view Medication-Assisted Treatment (MAT) as a form of pharmacotherapy that serves as a harm reduction tool when used in conjunction with counseling and behavioral therapies. MAT is effective at diminishing cravings, reducing high-risk behaviors associated with substance abuse, and creating stability for clients during transitional periods. MAT is not a life-long sentence – it can be used safely for extended periods of time or utilized as a short-term intervention for individuals struggling to remain abstinent. MAT when coupled with clinician-recommended counseling such as individual Psychotherapy, and Cognitive Behavioral Therapy, and group and social support help patients in various ways.
The mantra of helping patients turn over a new leaf rests on our philosophy that acknowledges and embraces the unique strengths, experiences, and needs that each person brings to the treatment process. It equips clients with the knowledge, life skills, spiritual tool kit, and emotional support to produce a meaningful character transformation necessary for sustained long-term recovery. Together we work diligently with our clients to uncover, discover, and discard; to unearth the authentic self in each client, healing the underlying causes of addiction. We provide the life-changing care that will empower men and women to overcome their dependence and addiction to opioids, address their mental health issues, and help them make the other changes that will support their successful pursuit of happier and healthier futures, free from the constraints of addiction.
For more information, please visit nldetox.com or contact 949-617-0719.
Sources
- NIDA. (). Real Teens Ask: What Are the Different Types of Opioids?. Retrieved from https://archives.drugabuse.gov/blog/post/real-teens-ask-what-are-different-types-opioids-0 on 2021, May 25
- National Institute on Drug Abuse. (2021, March 11). Opioid Overdose Crisis. Retrieved from https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis
- Substance Abuse and Mental Health Administration. (2021). National Survey on Drug Use and Health (NSDUH). Retrieved May 25, 2021, from https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health
- Luthra, S. (2020, April 24). Vaping, Opioid Addiction Accelerate Coronavirus Risks, Says NIDA Director. Retrieved from https://khn.org/news/vaping-opioid-addiction-accelerate-coronavirus-risks-says-nida-director/
- New Leaf Detox & Treatment. (2021, May 05). A Mosaic of Loss & How to Stem Opioid Relapse and Overdose Deaths. Retrieved May 25, 2021, from https://nldetox.com/mosaic-of-loss-opioid-relapse-overdose/
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep 2021;70:202–207. DOI: http://dx.doi.org/10.15585/mmwr.mm7006a4
- CDC. (2021, March 11). 2017-2018 Synthetic Opioids Overdose Data. Retrieved from https://www.cdc.gov/drugoverdose/data/synthetic/overdose/2017-2018-synthetic-opioid-overdose-data.html
- Drug Policy Alliance Headquarters. (n.d.). 10 Facts About Synthetic Opioids (Fentanyl). Retrieved May 25, 2021, from https://drugpolicy.org/drug-facts/synthetic-opioids-fentanyl
- Mayo Clinic. (2018, February 16). Am I vulnerable to opioid addiction? Retrieved from https://www.mayoclinic.org/diseases-conditions/prescription-drug-abuse/in-depth/how-opioid-addiction-occurs/art-20360372
- Maxwell, C. J., Bill, J. M., & Kate, L. L. (2020). Recent Trends in Cannabis Use in Older Americans. Annals of Internal Medicine, 174(1), 133rd ser. doi:10.7326/M20-0863
- Drug Enforcement Administration. (2019, September). Fentanyl (Trade Names: Actiq®, FentoraTM, Duragesic®). Retrieved from https://www.deadiversion.usdoj.gov/drug_chem_info/fentanyl.pdf
- NIDA. 2021, May 13. Overview. Retrieved from https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/overview on 2021, May 25
- NIDA. 2020, May 27. Prescription Opioids DrugFacts. Retrieved from https://www.drugabuse.gov/publications/drugfacts/prescription-opioids on 2021, May 25
- NIDA. 2021, April 13. Overview. Retrieved from https://www.drugabuse.gov/publications/research-reports/heroin/overview on 2021, May 25
- Nuwer, R. (2020, July 10). Americans Increase LSD Use—and a Bleak Outlook for the World May Be to Blame. Retrieved from https://www.scientificamerican.com/article/americans-increase-lsd-use-and-a-bleak-outlook-for-the-world-may-be-to-blame1/
- United States Drug Enforcement Administration. (n.d.). Fentanyl. Retrieved May 25, 2021, from https://www.dea.gov/factsheets/fentanyl
- NIDA. 2019, January 17. Treatment Approaches for Drug Addiction DrugFacts. Retrieved from https://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction on 2021, May 25
- Forum, A. P. (2019, October 10). Substance use disorders take a toll on more than just health. Retrieved from https://www.addictionpolicy.org/post/substance-use-disorders-take-a-toll-on-more-than-just-health