"The last time I thought about taking heroin was yesterday. I think of places I could score. But even as I spin this beautifully dreaded web I am reaching for my phone. I call someone, not a doctor or a sage, not a mystic or a psychic, just a bloke like me, another alcoholic, who I know knows how I feel. Constant vigilance is key because the disease of addiction is not rational."
- Russell Brand, 18 Years Sober
Addiction to alcohol and substances is a chronic medical disease marked by complex interactions and collisions between genetics, brain circuits, individual like experiences, and the environment. Though treatable like other chronic diseases such as asthma and diabetes, the variety and complexity of triggers and interactions involved in addiction, make abstinence, and full recovery without relapse, a challenging enterprise.
It also demands a commitment to current evidence-based methods of managing addiction, and a willingness to explore and consider new and experimental advances in relapse prevention.
In the cycle of recovery, the treatment phase is frequently an enriching, stimulating experience. Residential and outpatient treatment in clinical settings are veritable safe havens free from alcohol and drugs.
Stripped from the family, community, and familiar culture and network of peers, co-users, enablers, and dealers with their own system of values, the recovering individual in treatment is able to imagine new possibilities.
Those grappling with alcohol and substance abuse disorders routinely flourish and thrive as they submit to the recovery process in treatment. When immersed in wraparound treatment and services, medication-assisted treatment, psychological and behavioral health modalities, therapeutic modalities, peer support, education, wholesome recreational activities; and nurtured by friendships forged through the common bond of addiction, the individual in recovery is able to reimagine, change, and reframe his/her relationship with alcohol and drugs. But leaving treatment elevates the avoidance of relapse into a battle for sobriety and survival.
Despite the mantra, “relapse is part of recovery,” that has been advanced by many in the field of addiction, and supported by the alarming statistics of relapse, a growing body of scholarship shows that relapse is preventable if those in recovery are given the gold standard of care in treatment, education, and post-treatment support during recovery. Yet, the reality is that relapse is often predictable and inevitable, because of addiction’s inextricable relationship with the brain.
Disclaimer: Only for fair use for educational purposes and illustration. We do not own the copyright to this video.
Understanding addiction within the framework of the brain will help dispel the biases, judgment, and opinions many of us have about addiction and relapse after treatment.
Advances in neuroscience reveal the complexity of the brain and the primacy of the brain in substance disorders. A healthy brain is like a full philharmonic orchestra that skillfully renders a grand symphony.
Similar to an orchestra’s musicians specializing in bowed strings; double bass brass instruments; woodwinds, drums, piano, harp, keyboards, as well as electronic instruments, the brain has hundreds of chemicals or neurotransmitters with unique properties. Akin to a seventy person orchestra, the brain is powered by 80 billion neurons and other cells.

Chemicals serve as messengers or neurotransmitters that allow communication between neurons, by crossing the gap or synapses between neurons. In a healthy brain, the alchemy of chemical and electrical processes work alone or in concert to control basic functions.
Each type of neurotransmitter has distinct qualities and functions; some inhibit action, others stimulate activity. Some are responsible for basic functions such as breathing and digestion, others for higher functions such as thinking, emotions, learning, and memory. Some communicate exclusively with muscles to stimulate physical activity, still, others influence a person’s reactions to external events including sounds, smells, and a myriad of sensory stimuli.
Hundreds of chemicals, a veritable pharmacy, inhabit our brain allowing it the ability to orchestrate the body to function and maintain homeostasis and equilibrium. The five major neurotransmitters are:
Regulates sleep and emotions, influences sexual desire and arousal, impacts appetite and digestion, and powers the motor and cognitive actions. It promotes happiness and postive feelings.
Frequently referred to as the “love” chemical because of its critical role in human relationships, social behavior, and intimacy. It is instrumental in relationship building and sexual, romantic, and familial bonding. Mothers in labor and during breast feeding release Oxytocin, as do lovers.
The neurotransmitter that gives us our mojo to focus and strive and find meaning and pleasure in our lives. It allows us to be strategic beings who think, learn, strives, ruminates, considers, and plan. It also regulates heart rate, sleep, mind, and pain.
Released in the body during stress and trauma, calming the nerves and making people alert, aroused, and nimble to address the stress-inducing event. It elevates focus and concentration and has a positive effect on mood. Deficits in this neurotransmitter can cause depression and ADHD.
GABA is a subduing neurotransmitter that inhibits or blocks activity in the brain and nervous system. The release of GABA calms negative moods, relieves anxiety and pain, improves sleep, and lowers hypertension. It also boosts the benefits of exercise by burning fat and increasing lean muscle growth.
These chemicals transmit from neurons through synapses to receptive neurons, and cascade and surge through the body during specific events, times, and experiences to address precise needs.
The addicted brain is a pale version of its powerful counterpart. Normal neurotransmission, function, and performance are disrupted by drug and alcohol abuse. In a healthy drug-free brain, neurotransmitters are banked in the synapse to facilitate neurotransmission after the first release. Drug use however either supercharges decreases neurotransmission.
Communications between neurons are disrupted by the cumulative use of drugs and result in profound and progressive changes in people’s thoughts, feelings, and behavior. Habitual drug use manipulates, alters, and disturbs the natural chemical and electrical processes in the brain.
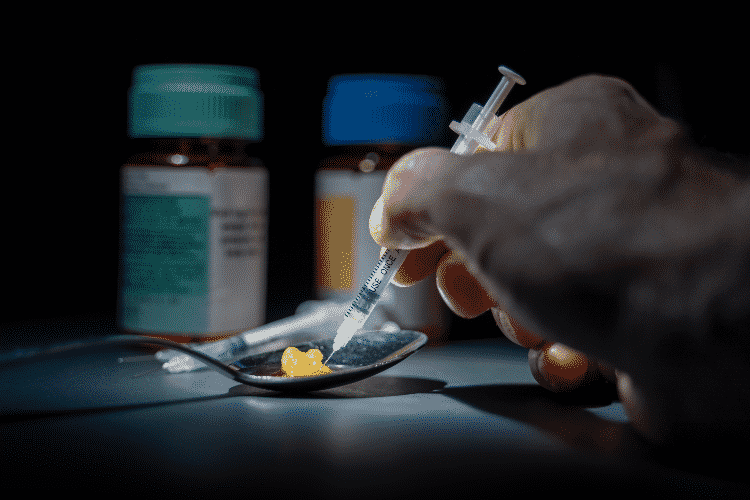
Drugs can disrupt one neurotransmitter while creating a cascading effect on other neurotransmitters by simulating the properties of naturally occurring chemicals in the brain. Both marijuana and nicotine attach to receptors and mimic neurotransmitters. Benzodiazepines alter the regular process neurotransmitters to elicit relaxation. Some drugs are dangerous and toxic to neurons.
For example, MDMA/Ecstasy/Molly damages serotonin delivering neurons to wipe out memory and recall. Meth use affects dopamine-releasing neurons and damage thinking and motor skills. The physical structure of neurons may also change with repeated use of substances.
Sobriety and relapse are influenced by a host of factors, unique to each individual, including the severity and duration of treated addiction, type of substance abused, mental and physical health, the environment the person striving for sobriety inhabit during recovery, the quality of treatment received, and the support systems available to patients after they leave treatment.

Though withdrawal is painful, sobriety immediately after treatment is easily maintained. However, the prevalence of alcohol in the larger society and in the reformed alcoholic's circles of influence, makes remaining sober a difficult task.

These highly potent drugs are extremely addictive and difficult to reject permanently without proper treatment and post-treatment support. The excruciating effects of withdrawal from this class of drugs that include bone pain, stomach cramps, nausea, and diarrhea, often compel a return to use and abuse.

Relapse rates among those who leave treatment are even higher than for heroin users, perhaps because it's a fast-acting drug that delivers quick, short intense bouts of euphoria. Though not physically addictive, meth is an extreme psychological addiction.

This expensive drug has connotations of elitism, luxury, and partying, without the attached stigma of street drugs or perception of junkies, that drive those in recovery to relapse. Though relapse is much lower than with heroin and meth, the frequency of cocaine use among those who relapse is high. Cocaine users incorrectly believe it is not an addictive drug but a social bonding agent.
Given the complexity of alcohol and drug addiction, and the powerful role of brain chemistry on this chronic disease, the occurrence of cravings and relapse after treatment is hardly surprising. Abstinence is achievable when someone is in a pure, sanitized bubble, far from conditions and environments that trigger a relapse. But relapse is an occupational hazard for those in recovery after they leave treatment.
In the larger environment where alcohol flows freely, is legal, and readily available, and drugs and other substances are easily procured, remaining sober requires vigilance, awareness, education, mindfulness, and psychological warfare. For those in recovery, the temptation to imbibe, ingest, and relapse is more pronounced when the general population indulges in alcohol and drugs as a part of ritualized fellowship, hospitality, and celebration. Few can remain detached while others partake in normalized cultural rites of drinking and drug use.
Craving for drugs after treatment is usually set off by internal triggers and external triggers, and cues from the past. Negative emotions such as fear, guilt, hate, and shame, and normal emotions such as boredom, nervousness, sadness, and embarrassment can make those in recovery vulnerable to a relapse.

External cues include seeing friends, family, and others from the past who participated encouraged, provoked, or enabled drug and alcohol use. Mere contact with these relics from the past can trigger an association with drug use, and create desire, longing, and craving in a newly sober person.
Revisiting places and attending events that were once the site of drug and alcohol consumption can also trigger cravings. Other major triggers are stress and anxiety, which can be managed with the behavioral tools learned in treatment. As sentient beings, people in recovery inevitably reflect on their past, which can evoke idealized visions of drug-fueled fun and carefree living. The mind and the body are inclined to remember the euphoria and serenity bought with drugs and alcohol while rejecting the pain and danger of past addiction. This trigger can lead to relapse if not managed through behavioral tools or addressed in therapy or support groups.
Relapse happens in a wave, gradually and then suddenly. Once a person in recovery responds to internal or external triggers, the waves roll in a sequence.

Emotional relapse is a reversal from the healthy behaviors learned in treatment to maintain sobriety. At this stage, individuals neglect self care, isolate themselves from others, skip or refuse to participate in meetings, and neglect good nutrition and sleep.

Mental relapse is the self-talk that rationalizes and glamorizes the use of drugs and alcohol, thinking about using, actively planning to score drugs or alcohol, dismissing the consequences of using, and embracing the idea that relapse is controllable and harmless.
Physical relapse is the final conclusion of emotional and mental dialogues resulting in obsessional compulsive thoughts about using, taking the plunge back into using drugs or alcohol, and gradually increasing use to the point of addiction,

Everyone in recovery is part of a tribe bound by a single narrative—the struggle to survive without alcohol or drugs, after falling into the pit of addiction. It is a hero’s and “shero’s” journey to self-actualization that can only be understood by others on the journey. As such, recovery is a communal journey. No one can remain sober or avoid relapse alone. It is a shared journey that requires us to open up, show our vulnerabilities and weaknesses, and ask for help and support when we need it.
To remain sober and safe may require us to reject the past, the site of our addiction, and reinvent ourselves in a tribe of like-minded people aspiring to be sober, and seeking to flourish and thrive in a drug and alcohol-free space.
The recovery community is vital around the globe with reach in every town, city, state, and country. A person striving for sobriety and trying to avoid relapse has many resources including AA and NA groups, sponsors, friends in recovery, therapists, groups, and phone and chat support. Surrounding ourselves with the resources available to us increases our chances of maintaining sobriety and avoiding relapse.
Overcoming addiction, abstaining from drugs and alcohol, staying sober, and being vigilant about avoiding relapse is a life long effort. It may be daunting and terrifying to think of never having a drink, or ingesting a drug, ever again for the rest of one’s life. But the person in recovery can reframe the goal on a daily basis by committing to stay sober just for that one day.
Renewing the commitment to stay sober the next day, and the next, and the next, ad infinitum become a way to abstinence. Attaining a day of sobriety on a daily basis adds up to a lifetime of sobriety, instead of focusing on the Herculean task of permanent sobriety which is too often elusive.
The field of addiction medicine is racing to produce drugs that prevent or decrease the chances of relapse. While experimental drugs submit to the rigors and hurdles of clinical trials, discoveries, longitudinal studies, and approval; the gold standard in current treatment offers evidence-based medical, behavioral, and social therapies.

At New Leaf Detox & Treatment, we are committed to meeting the needs of our patients with the most advanced best practices in addiction medicine and treatment and evidence-based standards of care, while always mindful of each client’s individual needs.
After extensive patient-provider engagement, careful screening, and medical and psychological evaluation, our clinician’s design individualized plans to meet each patient’s specific needs. The plans are comprehensive in scope using a variety of treatment modalities from our cornucopia of specialized care plans that include Medication Assisted Treatment.
New Leaf’s Medication Assisted Treatment plans for best client outcomes to feature three of the four FDA Approved MAT drugs: Buprenorphine, its extended-release injection Sublocade, and Naltrexone. These three MAT regimens and protocols have high success rates for clients when complemented with counseling and psychosocial support.
The patient begins cognitive-behavioral treatment with an individual therapist as well as in groups with a counselor to address the whole host of issues afflicting the patient, including anxiety disorders. Psychotherapy plans and specific treatment modalities tailored for the patient include individual counseling, group counseling, anxiety focused therapy groups, and process groups and activities.
The primary clinician and individual therapist and group counselor work in concert to treat the patient by resolving the underlying issues that led to addiction, followed by a variety of custom treatments that fortify the patient, clinical assessments throughout the process, and a considered discharge plan. Peer support, onsite medical assistance, family involvement, and post-treatment follow up support are part of New Leaf’s standard of care.
Send us your information and receive a free verification of benefits. All submitted forms or phone calls are completely confidential.
New Leaf Detox and Treatment
63 Mallorca, Laguna Niguel,
CA, 92677
866-932-0905